“Gout isn’t just your grandfather’s condition anymore.” – Leading rheumatologists warn as social media floods with stories of young adults battling sudden joint pain and skyrocketing uric acid levels. This article reveals how modern lifestyles are redefining gout’s demographic profile.
1. Rising Prevalence Among Youth
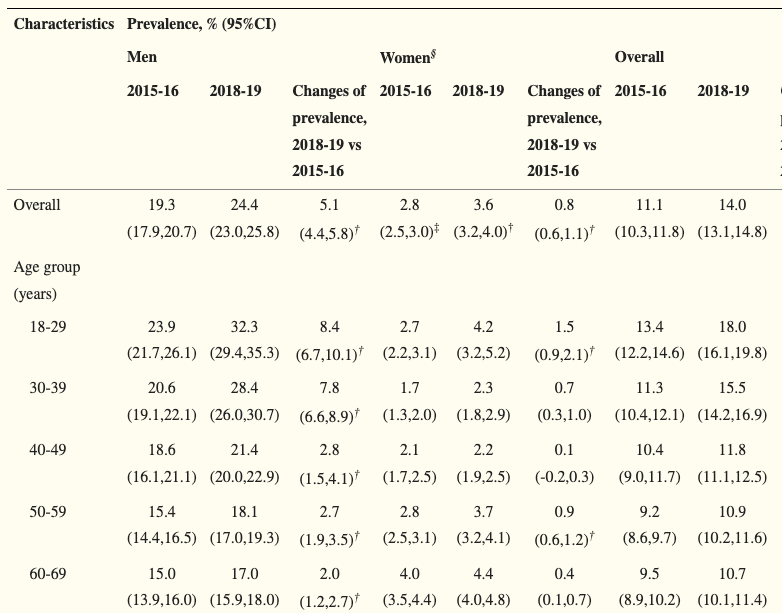
Hyperuricemia cases have exploded in recent years. In China, adult prevalence surged from 11.1% in 2015 to 14.0% in 2018, with young adults (18-29 years) comprising 32.3% of cases. Global trends mirror this shift, driven by dietary changes and sedentary lifestyles.
Key Drivers
- Dietary habits: Excessive sugary drinks, processed foods, and alcohol consumption
- Lifestyle factors: Sedentary behavior, prolonged sitting, and irregular sleep patterns
- Genetic predisposition: Family history accounts for 23.9% of uric acid variability
2. Understanding the “Pain” Behind Gout
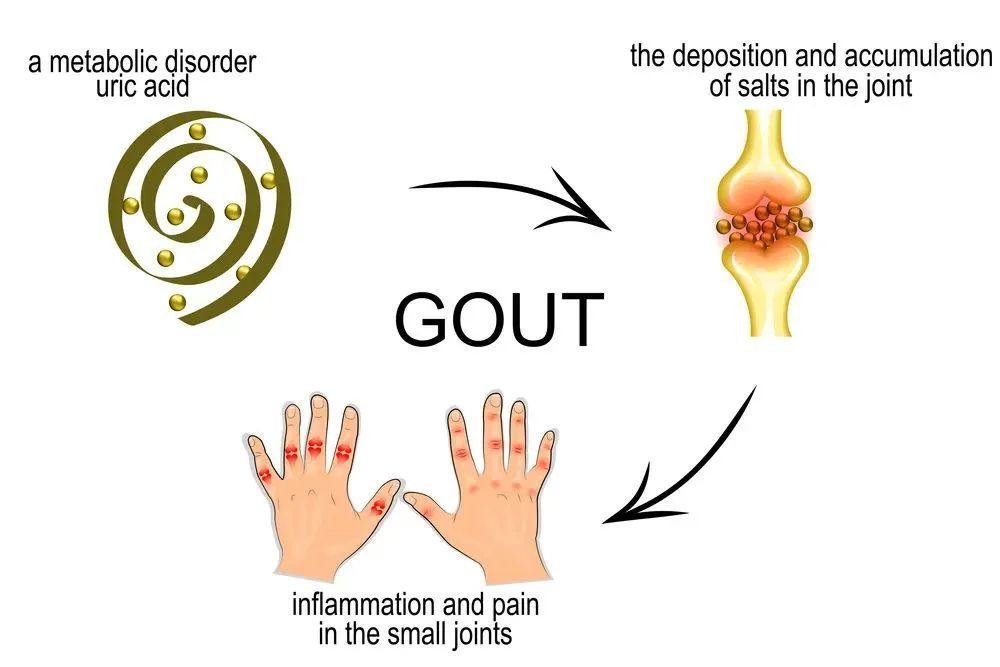
Gout pain originates from urate crystals forming in joints when blood uric acid exceeds normal levels. These sharp crystals trigger intense inflammation and excruciating pain. Historically, 17th-century physician Thomas Sydenham described gout agony as “unbearable even to bedsheet touch.” Modern patients compare flare-ups to “hammer strikes” when air touches affected joints.
Complications
- Tophi: Untreated gout causes crystal clusters under skin, leading to deformities and infections
- Joint damage: Chronic inflammation erodes cartilage and bone structures
- Systemic risks: Associated with kidney stones, cardiovascular disease, and diabetes development
3. Beyond Diet: Lifestyle Factors Fueling Gout
While purine-rich foods (red meat, seafood) affect uric acid, 80% of purines originate internally through cell turnover. This makes lifestyle choices critical:
Critical Risk Factors
- Alcohol: Beer and spirits impair kidney excretion, raising uric acid levels
- Sugary beverages: Fructose boosts uric acid production
- Obesity: Excess fat promotes inflammation and insulin resistance
- Dehydration: Inadequate water intake reduces uric acid clearance
Myth Busting
- Dietary purines only contribute 20% of uric acid
- Strict low-purine diets show limited impact (≤0.3% reduction)
- Healthy plant proteins like beans, lentils, and tofu protect joints
4. The Treatment Compliance Dilemma
Despite severe pain, 60% of patients fail to follow long-term urate-lowering therapy (ULT). Common reasons include:
- Believing diet alone controls gout
- Fearing medication side effects
- Skipping follow-up appointments after pain subsides
2022 NICE Guidelines
- First-line ULT: Allopurinol or febuxostat to maintain uric acid <6 mg/dL
- Annual blood tests even after target levels achieved
- Focus on balanced nutrition over restrictive diets
5. Sustainable Uric Acid Management Strategies

Effective gout control requires a comprehensive approach:
Dietary Adjustments
- ✅ Hydrate: 8-16 glasses of water daily
- ✅ Dairy: Low-fat milk/yogurt promotes excretion
- ✅ Vitamin C: Citrus fruits lower uric acid
- ❌ Avoid: Alcohol, organ meats, high-fructose corn syrup
Lifestyle Changes
- Exercise: Swimming reduces obesity and inflammation
- Sleep: 7-9 hours nightly regulates metabolic health
- Stress management: Chronic stress worsens inflammation
6. Why Youth Are Particularly Vulnerable
Young adults face unique challenges:
- Convenience foods: Reliance on takeout and sugary snacks
- Alcohol culture: Social drinking exacerbates uric acid buildup
- Sedentary jobs: Desk-bound work reduces physical activity
Case Study
A 17-year-old with obesity and frequent fast-food intake developed gout after years of unchecked habits.
7. A Wake-Up Call for Systemic Health

Gout signals broader metabolic dysfunction. Elevated uric acid correlates with:
- Diabetes: Each 1 mg/dL increase raises diabetes risk by 20%
- Heart disease: Chronic inflammation accelerates atherosclerosis
- Kidney damage: Uric acid crystals impair renal function
Proactive Steps
- Regular health screenings for uric acid, blood pressure, and cholesterol
- Early intervention with ULT to prevent irreversible damage
Conclusion

Gout is no longer an “old age” ailment. Young adults must prioritize metabolic health through balanced diets, active lifestyles, and medical guidance. Understanding uric acid science and adopting sustainable habits reduces flare-ups and safeguards long-term well-being.
References
- Data on hyperuricemia prevalence
- Clinical insights from rheumatologists
- NICE guidelines
- Dietary recommendations
- Alcohol and gout risks
For more detailed guidelines, consult healthcare providers or visit authoritative sources like the National Institute for Health and Care Excellence (NICE).
